Endometrial Hyperplasia
How to deal with this precancer condition of uterus. The modern approach.
Unlike my other write-ups, this one is rather more specialized. Probably you are reading this if you or your near and dear ones have been diagnosed with endometrial hyperplasia and waiting for the next step of treatment. You've come to the right place.
ℹ️ For the clarity of information.
I would like to divide into 3 groups of women
☝🏾 Group A:
Women who have been diagnosed to have endometrial hyperplasia on a biopsy and still has got their uterus inside. This writing is mostly for this group.
✌🏾 Then Group B:
Women who have been diagnosed with endometrial hyperplasia after they had uterus removal surgery or hysterectomy.
If it is a simple hyperplasia or hyperplasia with atypia, then your treatment is likely complete, but you should discuss that with your gynecologist. You don't really have to read this. However, for general knowledge, you are welcome to read.
🤟🏾 Group C:
I guess there could be a 3rd group of women where the uterine endometrial hyperplasia has been diagnosed on ‘ultrasound scan’. Well, this cannot be diagnosed with certainty with an ultrasound scan. However, sometimes some reports mention this. If you just had ultrasound and not had the biopsy yet, you need at least a camera test inside the uterus (Hysteroscopy) and get a biopsy from the inside lining of the uterus.
🚗 💭💭 Let's start…………
🤷🏻♀️ What is endometrial hyperplasia?
Endometrial hyperplasia is too much of cell-divisions within the inside lining of the uterus. And the inside lining or endometrium is getting thicker. Why understanding of hyperplasia is important? This is because this is the pre cancer stage, before progressing into uterine cancer.
Again, endometrial hyperplasia is divided into 2 different groups, as evident under microscope.
First is endometrial hyperplasia without atypia and 2) another is atypical endometrial hyperplasia.
🤔 What is ATYPICAL endometrial hyperplasia?
👨🏻⚕️ Atypical endometrial hyperplasia is more interesting. If we look deeper into the uterus, we will find in 50% cases, that is, every second individual, have already developed endometrial cancer. It was not picked up in the biopsy and this time the biopsy only picked up endometrial hyperplasia with atypia. So atypia is something to watch out for, on the biopsy report.
🫣 How hidden cancer can be missed?
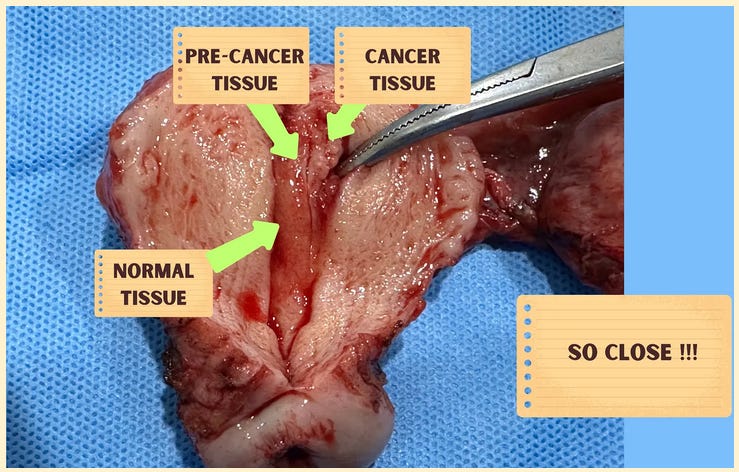
I am sure you are asking if there is hidden cancer why this was not reported? And only ‘atypia’ was reported instead?
Well, the human body is complex. I will show you a picture here.
You can see when cancer develops inside the uterus, the whole uterus doesn’t become cancerous all of a sudden. Instead, cancer starts at the corner or corners, and eventually it involves the whole of the uterus. Hence, even if cancer has started within the uterus, some of the biopsy reports will be normal or just show pre cancer, as the sample was from the neighboring tissue of cancer.
As a matter of fact, cancer is hiding somewhere else. While taking the biopsy, it is the gold standard to watch inside the uterus. As we take directed and targeted biopsy.
🧑🏻⚕️ Treatment
Anyway, if a pre cancer has been identified, what is the next step? Of course, the next logical step will be to remove the uterus. This will completely stop the progression into cancer. And of course, if it is an early cancer, with the surgery you will remove it. End of story!
🥗 By diet, exercise and avoiding bad chemicals
However, there are some recent data which suggest that if we can remove the causative factor or the factors which caused the extra cell division of the inside lining of the uterus in a good number of cases, patients can avoid having a surgery. Uterus will get back to normal endometrium.
❓❓ What causes endometrial hyperplasia?
Moving forward, let's address the next point. What causes endometrial hyperplasia?
Mostly it is a hormone mismatch. Too much of Oestrogen. That means because of extra body weight, extra fat cells convert many chemical in to a female hormone called oestrogen. Too much of oestrogen drives crazy cell divisions within the inside lining of the uterus. Uncontrolled cell division is precancer and cancer. Normally cells divisions can be stopped and body can place a brake. But in cancer that break fails and tumour develops.
Losing weight through a proper diet and exercise can help normalize hyperplasia.
Occasionally we will find patients who take too much of plant-based estrogen containing diet such as soybean. Some might have taken too much of estrogen tablets in the body for hormone replacement therapy.
In either of the cases, the body gets too much of oestrogen. Oestrogen talks to both uterus and breast. These organs are hormone sensitive. Oestrogen can drive cancer in both the organs.
👨🏻⚕️ Sometimes extra estrogen may also come from some group of chemicals in our environment called EDC (Endocrine Disturbing Chemicals) This could be pollutants from air water or cosmetics. Could be dairy products in unregulated countries and economies where chicken is injected antibiotics and hormones for cheap meat. Could be the cows those are injected estrogen to yield higher amount of milk for bigger profit.
A breast cancer treatment medicine tamoxifen can also cause hyperplasia. In this case, you need to consult the breast cancer doctor to change tamoxifen.
Well, if you can revert all those factors, then endometrial hyperplasia could be reverted. However, after 6 months, we will need to perform another biopsy to check if the endometrium has returned to normal. If patients’ diet and lifestyle modifications were successful.
💊💊Treatment By Progesterone
Some women will choose to have a progesterone hormone against hyperplasia. Progesterone is another female hormone, and it protects the endometrium from developing into cancer and somehow counteracts the effects of estrogen. Here, the patient may choose to have oral progesterone tablets or a local progesterone therapy inside the uterus.
Oral progesterone (tablets) will travel through liver before going to uterus and can damage liver. After 35 years if age, liver damage from hormones is higher. Hence, a more clever approach is to give local progesterone inside the uterus. Here, the progesterone acts directly on the inside lining of the uterus and dials down the pre-cancer endometrium into normalcy.
📝 Checking result of treatment
Following 6 months of treatment, it is important to verify if the endometrium has fully recovered. Otherwise, a more rigorous, potentially surgical, approach may be necessary.
This 6-month follow up must be with a biopsy, not just by checking the amount or pattern of the bleeding, or just by doing ultrasound to check inside lining thickness.
We must not forget we are dealing with a precancer condition.
✂️ Definitive surgery- hysterectomy
This brings us to the surgical treatment of endometrial hyperplasia.
This is by uterus removal surgery. Generally, this is a hysterectomy. Depending on patients’ age, the ovaries and fallopian tubes might also need to be removed.
If someone has developed endometrial hyperplasia with atypia, then just lifestyle changes or getting progesterone might be more risky.
✂️ Laparoscopy surgery
👨🏻⚕️ Patients with atypia needs to be offered to have uterus removal surgery. As in half of the cases with Atypia, we will find uterine cancer has already developed within the uterus. Don't worry, in most cases, uterus removal can be done through a keyhole surgery called laparoscopy.
💁🏻♀️ Let’s conclude
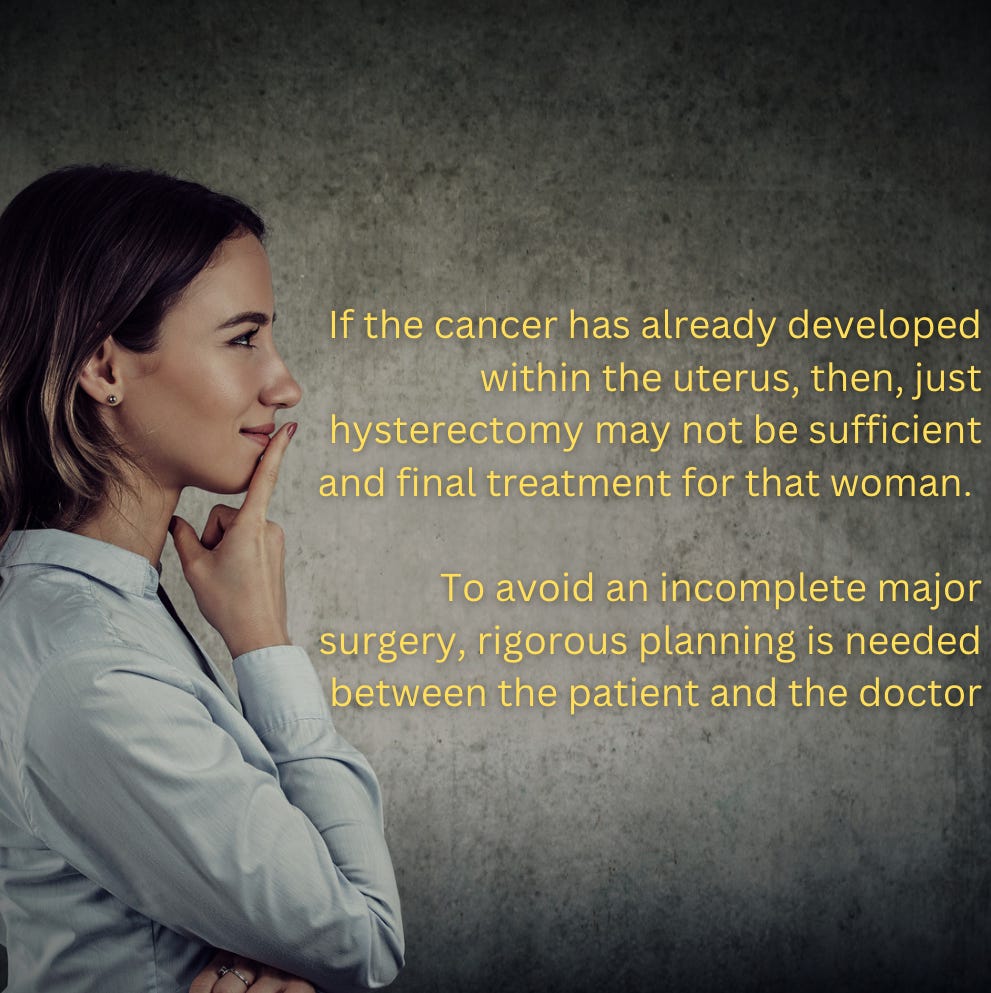
Doctors, will need to be vigilant to check if the cancer has already developed within the uterus. Because in those cases, just hysterectomy may not be sufficient and final treatment for that woman. To avoid a second major surgery, rigorous planning is needed between the patient and the doctor, just so that the patient can get the benefit of the scientific advances of modern gynecology.
Endometrial cancer rates are rapidly rising, but fortunately, treatment is also improving significantly. In summary, endometrial hyperplasia is increasingly common. With proper treatment and planning, the patient can go home happy and potentially live happily ever after.
(এই টপিকের বাংলা লিংকের জন্য এখানে ক্লিক করুন)
(The English version of this topic is above page itself)
This is an impartial , unsponsored health information. For public awareness and not a replacement of Medical Advice.
Search tool: Endometrial hyperplasia Pre-Cancer Biopsy Hysteroscopy Targeted Biopsy Estrogen Progesterone Fat Cells HRT EDC Tamoxifen Laparoscopy Hysterectomy